With an estimated worldwide incidence of 570,000 cases and 311,000 deaths in 2018, cervical cancer ranks as the fourth most frequently diagnosed cancer and the fourth leading cause of cancer death in women. It is projected that 1,350 cases of cervical cancer would be diagnosed in Canada in 2020, making it the 13th most commonly diagnosed cancer among females. More than 70% of cervical cancers diagnosed are in the age group between 18–39 years. In cases where surgery is not possible, the curative-intent treatment for locally advanced cervical cancer (LACC), involves a multimodality approach that includes a combination of external beam radiotherapy (EBRT) with concurrent chemotherapy followed by brachytherapy (BT). The EBRT treatment is applied to the pelvic lymph nodes, parametria, and primary tumor, to a dose adequate to control the microscopic disease. The addition of BT serves to boost the gross tumor and improves disease control and survival.
In locally advanced cervical cancer (LACC) treatment, brachytherapy (BT) remains the gold standard for boosting to curative doses of radiotherapy. Progress towards balancing target and routine tissue dosimetry, for better clinical outcomes, has been made possible by using MRI-guided imaging to improve volumetric treatment planning. These building blocks enable adaptation to the patient’s anatomy and tumor geometry. Further evolving from the original “one size fits all” approach towards truly patient-specific BT delivery requires improvements along the entire BT care treatment pathway. From the pre-insertion applicator selection to the post-insertion treatment plan optimization, multitude factors need to be optimized that are patient specific in order to improve the outcome of the treatment.
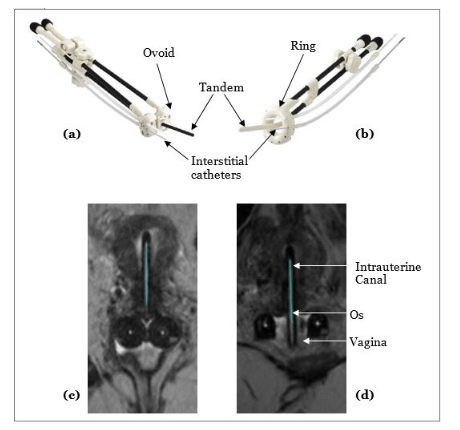
BT involves the placement of a radioactive source very close to or inside the tumor to help deliver a high radiation dose to the tumor. In North America, BT for cervical cancer is delivered as high-dose-rate (HDR; fractionated high dose rate treatments delivered daily or weekly) or pulsed-dose-rate (PDR; low dose rate hourly treatments delivered over a few days) treatments, both of which appear to be relatively equivalent treatments in terms of survival outcomes based on existing retrospective and prospective studies. BT for cervical cancer can be performed using intracavitary (IC), interstitial (IS), or a combination technique (IC/IS). Figure 1a and Figure 1b shows the two most commonly used IC applicators. The vaginal component (ring and ovoids) sits in the upper part of the vagina, i.e., close to the cervix, and the tandem passes through the internal orifice of the cervix uteri into the intrauterine canal (Figure 1c and Figure 1d). The radioactive source travels through these applicators to treat the upper vagina, cervix, and uterus. IS catheters (small tubes) are placed in and around the residual disease, anchored using the vaginal component, to achieve better lateral dose coverage. The choice of the applicator and the technique depends primarily on the disease extent and patient anatomy, a decision made based on information obtained from images, mainly MRI, acquired post-EBRT.
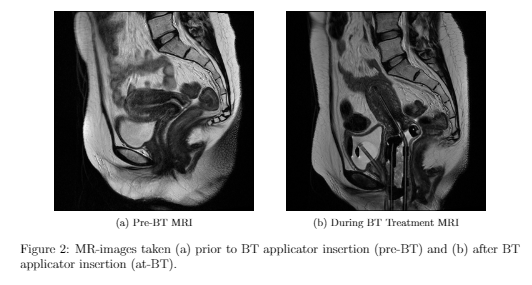
One of the technical advancements in cervical cancer treatment involves the use of image guidance using magnetic resonance imaging (MRI) in BT for better visualization of the tumor and surrounding critical structures. This leads to better dose optimization and could improve treatment outcomes. To assist in this BT process, two MRI scans are done: one close to or at the end of EBRT (pre-BT) and one after BT applicator insertion (at-BT) as shown in Figure 2. Before selecting and inserting an applicator, the physicians make several educated predictions, mainly based on the pre-BT MR images to determine the most plausible uterine/cervix deformation that would result from a given intrauterine tandem. However, with large distortions caused by the applicators, such speculation to guide implant strategy is far from accurate and cannot systematically prevent sub-optimal dosimetry post-insertion. Hence, the aim is to build predictive models to guide BT processes and decisions, to improve the efficiency and quality of BT in LACC.
For more information on this project please communicate with Shrimanti Ghosh